Why are South Asians more likely to be diagnosed with Type 2 diabetes?
By Angad Deol
Growing up as a member of the South Asian community, hearing about my family members’ diagnoses of Type 2 diabetes was unfortunately a common occurrence. Type 2 is the strain of diabetes where insulin production is reduced and a lack of cell response leads to increased blood sugar levels.
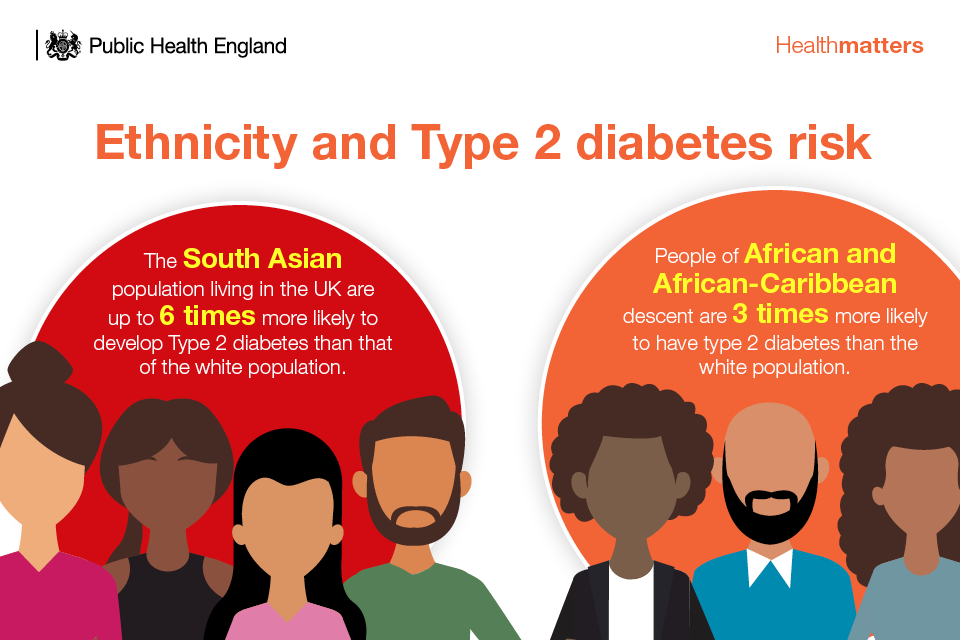
South Asia — especially India — has become a global hotspot for diabetes. Indians who migrate to other regions of the globe also show higher rates of diabetes compared to other ethnic groups. A great deal of research has been performed to investigate this occurrence, mostly looking at biological factors; however, emerging research into lifestyle and social determinants of health has begun to provide more insight.
Biological factors
The South Asian community faces a greater risk of insulin resistance, which is when the cells of your muscles, liver, and fat do not respond correctly to insulin, meaning you have to produce more of it. On a large scale, healthy and young Indian adults have a greater prevalence of insulin resistance than other ethnic groups. It should be noted that insulin resistance is associated with other risk factors such as high blood pressure, greater body fat percentage, and high triglycerides.
Body composition also affects the risk of developing diabetes. South Asians tend to have higher amounts of body fat — in particular, subcutaneous and visceral fat. Visceral fat is especially bad since it produces inflammatory cytokines — molecules that play a role in immune responses — an overabundance of which can cause a risk of cardiovascular diseases and indirectly lead to higher blood pressure.
Social, environmental, and lifestyle factors
Science has evolved over time, and it is clear now that underlying determinants of health play a role in how diabetes develops in South Asian communities.
Urbanization and migration especially have factored into the skyrocketing rates of diabetes within South Asian populations. For example, the populations of urban regions of India have a greater prevalence of diabetes compared to rural regions, with rates in Southern India being almost double in urban centres compared to villages. However, as time has progressed, even villages have shown increased rates of diabetes. More widespread adoption of sedentary lifestyles in urban environments is likely the leading cause.
In an interview with The Varsity, Ananya Tina Banerjee, an assistant professor at the Dalla Lana School of Public Health and the Faculty of Kinesiology & Physical Education, spoke about the effects of migration on the rates of diabetes in South Asians. Banerjee affirmed the notion that migration has been a potential risk factor for diabetes, explaining that it was because “certain South Asian subgroups undergo significant higher stress — attributable in part, to the social, economic and political marginalization of immigrants and refugees.”
She added that this higher stress load leads to greater food insecurity, less access to physical activity opportunities. The experiences of systemic racism and low social support in South Asian migrant communities also contribute to this stress — and all together, these factors can partially explain the greater risk of diabetes in South Asians.
When asked about the role that colonialism may have played in the emergence of a diabetes epidemic in South Asians, Banerjee said that “colonialism as a structural risk factor for the diabetes epidemic in South Asia has not been largely explored.”
“There is [a] need to understand how Eurocentric diets, illnesses and economic practices [that] were imposed by the British in South Asia during the colonial era disrupted lifestyles, traditions, and even languages,” said Banerjee. “These colonial practices are likely to continue to detrimentally affect communities living in South Asia.”
The Varsity also spoke to Leanne De Souza-Kenney, an assistant professor in the teaching stream at the Department of Human Biology and the Health Studies program at University College. De Souza-Kenney noted that dietary choices and physical activity both play a significant role in the development of diabetes in many communities, including the South Asian community.
“While there is a genetic predisposition to certain conditions like diabetes, this can be addressed by reducing environmental exposures and risk factors for diabetes. Understanding the social determinants of health and the exposures to risk factors for disease states is critical for populations to learn about.” De Souza-Kenney added.
How can we intervene?
Both De Souza-Kenney and Banerjee offered their opinions on potential interventions that could begin tackling the diabetes problem in South Asian communities.
“We need a diverse array of effective changes in policies and the environments in which South [Asians] live, work, and play,” Banerjee said. Doing so, she believes, would be a good start to mitigating the diabetes epidemic, since it would tackle the root causes of inequities in health. Banerjee believes that these changes can be reached through improving access to resources and preventative services within communities, as well as promoting policies that improve the care and management of diabetes.
De Souza-Kenney added that health literacy and patient education are places to start, and that we should start by creating a safe environment for discussion. “The conversation should be just that — an exchange that invites people to play an active role in their health outcomes, rather than a one-directional listing or reprimanding, or dictating incongruent recommendations to how people live their lives,” she said.
Education is a big part of promoting access to health care, according to De Souza-Kenney. “Education includes helping affected or vulnerable populations to learn what to look for and when to seek help, as well as [the value] of tests and opportunities like screening measures.” She believes that those who are at risk for Type 2 diabetes mellitus due to factors such as family history and environmental exposures should feel supported and should have the opportunity to educate themselves on the importance of screening tests and self-monitoring blood glucose.
From : Varsity












Facebook Comments